Epiretinal Membrane
What is an Epiretinal Membrane?
The macula is the special area at the center of the retina, which is responsible for clear, detailed vision. The macula normally lies flat against the back of the eye, like film lining the back of a camera. An epiretinal membrane is a condition where a thin sheet of scar tissue grows on the surface of the retina. This scar tissue can contract causing the macula to become wrinkled and may result in swelling of the retina and vision changes. This condition is also known as “macular pucker”, “cellophane maculopathy”, or “premacular fibrosis”.
What Causes an Epiretinal Membrane and who is at Risk?
Epiretinal membranes typically occur in those over age 50. They are often related to the degeneration of the vitreous, a normal aging process inside of the eye. As the vitreous to pulls away from the retina a scar-like tissue may develop. If this scar-like tissue contracts, it can causes the retina to wrinkle or pucker. Many other eye conditions can be associated with the formation of an epiretinal membrane including trauma, diabetic retinopathy, retinal tears, prior retinal detachment, and ocular inflammation (uveitis). The condition can affect both eyes in approximately 25% of cases.
What are the Symptoms of Epiretinal Membrane?
The condition is mild in most cases with very few symptoms. In more severe cases the vision becomes blurred and distorted, just as one would expect a picture to appear distorted from a camera with wrinkled film. Straight lines, like doorways or telephone poles, often appear wavy. Vision loss can vary from barely noticeable to severe. For most people, vision remains stable and does not get progressively worse.
How is an Epiretinal Membrane Diagnosed?
Your retina specialist can detect macular pucker by examining your retina using a dilated eye exam. A retinal scan called and optical coherence tomography (OCT) is used to document how extensive the scar tissue is and can help provide information about how much retinal damage exists (figure 2). OCT can also be used to follow the growth and contraction of the epiretinal membrane and its response to treatment. A photographic test called a fluorescein angiogram may be done in order to tell the extent of damage to the macula. This technique is also useful for evaluating possible underlying causes of an epiretinal membrane.
How is an Epiretinal Membrane Treated?
Treatment is not necessary if symptoms are mild. When an epiretinal membrane causes vision loss or the symptoms start to interfere with a persons normal daily activities then surgery is recommended. Vitrectomy surgery is the only treatment for effectively removing the membrane and improving the symptoms. During this procedure micro-forceps are used to gently remove the membrane that is wringing the macula. Following removal of the membrane, the retinal architecture usually returns to a more normal state and the symptoms slowly improve (figure 3). Approximately 80-90% of patients have improvement in blurred vision and distortion, though the vision usually does not return all the way to normal.
What is the long-term impact of an Epiretinal Membrane on my vision?
Approximately 90% of epiretinal membranes do not grow or cause progressive blurring or distortion of vision. Mild epiretinal membrane is causing only minimal symptoms typically do not progressively get worse. In the 10% of cases where the epiretinal membranes causes a progressive decrease in vision, the vision loss can be profound and permanent without treatment. Once the epiretinal membrane has been surgically removed the vision is typically stable. It is unusual for an epiretinal membrane to reoccur once it has been removed.
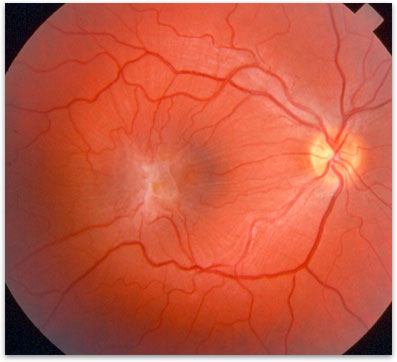
Figure 1. Epiretinal Membrane overlying the retina.
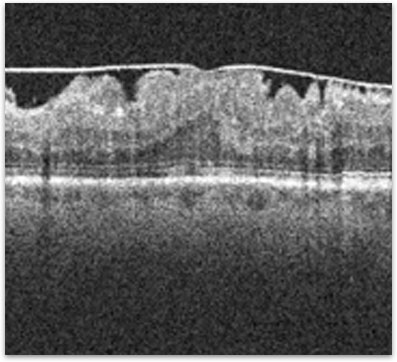
Figure 2. High resolution OCT of a macula showing the overlying epiretinal membrane (arrows) and macular thickening.
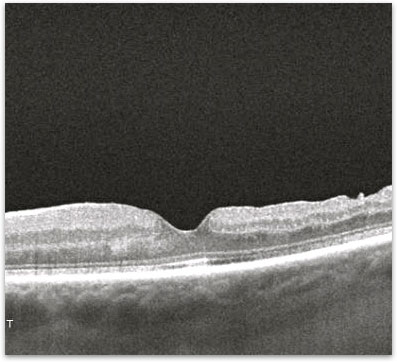
Figure 3. Appearance of a macula with an epiretinal membrane after surgery.