Macular Hole
What is a Macular Hole?
The retina is the layer of tissue that lines the back of the eye that senses light. The macula is the part of the retina that is responsible for your detailed vision and lies in at the very center of the retina. A macular hole usually develops in the center of the macula at the central point of vision (figure 1).
What causes a Macular Hole and who is at risk?
A macular hole develops when the vitreous gel that normally fills the eye begins to age and pulls away from the macula. As the vitreous gel pulls away from the macula it exerts traction that can result in the formation of an opening or hole in the central vision. Over time the macular hole can enlarge causing further worsening of the vision. For reasons not fully understood, the condition is more common in females and typically occurs around age 50 or 60. The second eye is affected in approximately 15% of cases.
What are the symptoms of a Macular Hole?
Early on when the hole first begins to form the central vision becomes blurry and distorted. Over time as the hole enlarges a blind spot forms blocking out the central vision and the vision may decrease such that that only the “Big E” is visible on the eye chart. In general, people do not go blind from macular holes. Even if surgery is not performed, typically the peripheral or side vision is almost always maintained.
How is a Macular Hole diagnosed?
Your retina specialist can detect a macular hole by examining your retina using a dilated eye exam. A retinal scan called an optical coherence tomography (OCT) is used to document the size of the macular hole and can help provide information about how much retinal damage exists (figure 2). OCT can also be used to follow a macular holes response to treatment. Occasionally a photographic test called a fluorescein angiogram may be done in order to further evaluate the condition of the macula.
How is a Macular Hole treated?
Vitrectomy surgery is typically the most effective treatment for repair of a macular hole. The vitreous is removed from the eye and replaced with a gas bubble. The gas bubble slowly dissolves and the eye fills with natural fluids over about 1-2 weeks. The patient usually must keep their faces down for a few days following surgery. This position allows the bubble to gently press against the macula and helps the hole to close. In very select situations where the macular hole is small and the vitreous gel is pulling on the edge of the macular hole an injection of medication in the eye may cause the hole to close without the need for surgery.
What about face-down positioning after surgery?
Face-down positioning is important as the success of the surgery often depends on how well this position is maintained. Fortunately the majority of macular holes close quickly, within a few days, especially smaller macular holes. If you cannot remain in a face-down position for the required period after surgery, vision recovery may not be successful. People who are unable to remain in a face-down position for a few days may not be good candidates for a vitrectomy. However, there are a number of devices that can make the “face-down” recovery period easier on you. The duration of face-down depends on your specific doctor's recommendations. There are cases for which no face-down is required at all.
What can I expect for my vision?
Successful closure of the macular hole with vitrectomy is very high, approximately 95-100%. Once the hole closes the vision typically slowly improves and any distortion decreases. The visual outcome typically depends on how large the hole was and on how long the hole was present before surgery. Most patients note less distortion and are able to read two to three more lines on the eye chart. Typically the vision does not return all of the way to normal.

Figure 1. Color Photograph of the macula showing the appearance of a macular hole.
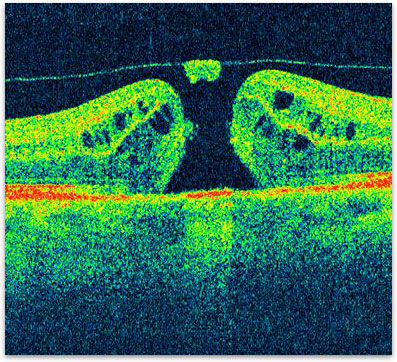
Figure 2. OCT showing the typical appearance of a macular hole.
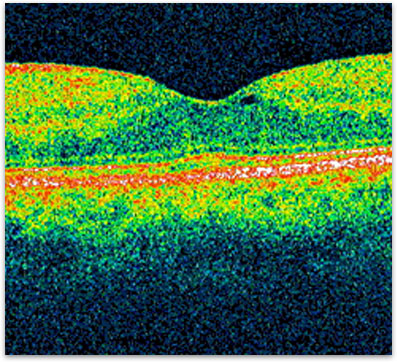
Figure 3. OCT showing the closure of the macular hole after surgery.